Parched for fresh cuisine: Life in food deserts
Graphic illustration by In-Depth Section
Food deserts are classified as regions with little access to fresh produce, and they affect millions of Americans.
November 9, 2021
Picture a desert: arid and empty, without water in sight. Similarly, food deserts are impoverished regions where immediate access to healthy foods is out of reach, and their prevalence affects millions of Americans.
The United States Department of Agriculture defines a food desert as an area where at least 33% of the population lives more than one mile in an urban area — or more than 10 miles in a rural area — from the nearest large grocery store.
“It’s not just about there being physical locations where people can access healthy food but also how reasonable it is for people to actually get there,” said Joanne Seavey-Hultquist, director of the CalFresh Healthy Living Program for the Santa Clara County Public Health Department.
Many other terms also describe a population’s access to food. These include food oases — areas with a high access to fresh produce like the Bay Area — and food swamps, areas with an abundance of junk food, convenience and liquor stores. Many food deserts are also food swamps, but food swamps have high junk food density, while food deserts define the scarcity of healthy ones. Also associated with food deserts, food insecurity describes places with limited access to food because of financial constraints.
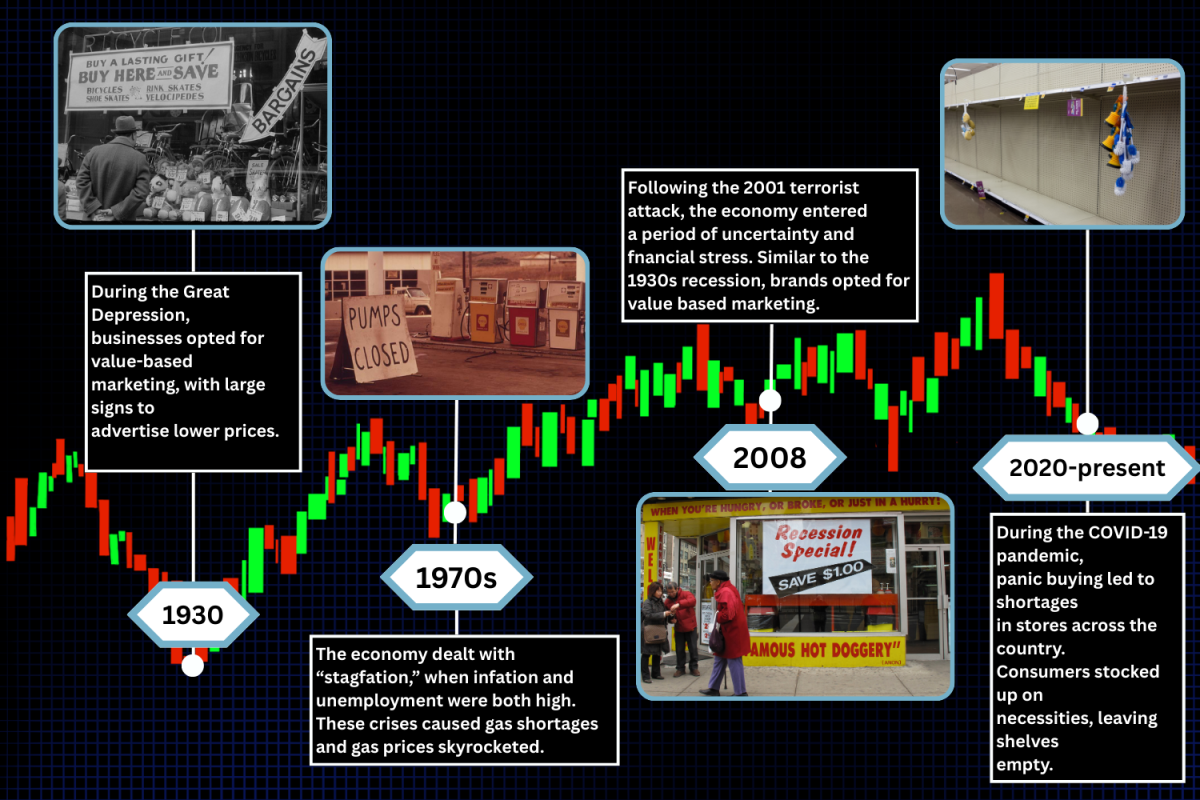
Between 2000 and 2006, the USDA identified approximately 6,500 food deserts; today, estimations show that more than 23.5 million Americans inhabit them. The Food Empowerment Project’s study of Santa Clara County concluded that low income communities were 14 times less likely to have access to even frozen food compared to higher income areas. Despite the problem’s prevalence, food deserts are not a sole cause.
Of the 23.5 million Americans inhabiting food deserts, 11.5 million have low incomes, and communities of color, mostly Blacks and Latinos, are disproportionately affected. The National Center for Biotechnology Information conducted a study on two low-income African American food desert neighborhoods in Pittsburgh, Pennsylvania that were suffering from food insecurity. The study found that from 2018 to 2020, while food insecurity in the nation increased by 60% due to COVID-19, the sampled neighborhoods saw an 80% increase, indicating a racial disparity of food insecurity between African American communities and the nation as a whole.
“I think it boils down to structural racism, in which we associate minority communities with oftentimes having higher rates of poverty,” said Matthew Landry, a postdoctoral research fellow in the Stanford Prevention Research Center. “And for a food store brand to want to build a store in that community, they’re going to want a number of households that can pay higher prices because that’s where they get the greatest sources of revenue.”
Other factors include an absence of public transportation, weak local economies, sudden shifts in population, gentrification, complicated geography and food insecurity. Food desert residents often cannot afford groceries because they are cash-poor, but another major hindrance is that they are time-poor. It is possible for some people to take a long trip to the store, but it is often not feasible for those who have to look after family members, work or perform other tasks. In some cases, groceries may have to be hand-carried over long distances, something that is problematic for large families.
At the start of the COVID-19 pandemic, food insecurity increased nearly 32.3%. This significant spike isolated already marginalized populations and greatly exacerbated the effects of food deserts. Greater unemployment levels have caused an uptick in food insecurity, shortened grocery store hours, decreased public transportation usage and increased food prices. Although online delivery systems may alleviate some issues, they are not options for many Americans who lack the internet, are unable to afford the delivery fee or live outside the delivery range. Research published by the CDC states that due to food insecurity and poor food quality from food deserts, Latino and Black populations were 4.7 times more likely to get infected by COVID-19 than Caucasians.
The consequences are dire for those without easy access to healthy food. Residents often stick to unhealthy food because they are cheaper and have a longer shelf life.
“After learning about food deserts and their effects on communities in the U.S., I don’t take the countless healthy options I have for granted anymore,” senior Melissa McCollough said. “It’s definitely important for your mental and physical health to eat healthy foods and fulfill nutritional guidelines.
A 2017 correlation study from the International Journal of Environmental Research and Public Health found that food swamps are good indicators of obesity and that the promotion of unhealthy diets in these areas leads to malnutrition, diabetes and cardiovascular diseases for many. Stores also encourage these unhealthy foods and entice consumers to purchase junk foods by putting candies, snacks and sodas by the cash register, where all shoppers will pass through before paying.
“There’s a very conscious effort by marketers to design stores just to tap people’s impulse buy,” Seavey-Hultquist said. “The CalFresh Healthy Living Program works alongside store owners and asks them, ‘Do you think you can put apples and bananas and pears at checkout?’ Because at the last minute, if people are impulse buying, we want them to impulse buy healthy.”
Additionally, residents in poor communities are commonly unable to get proper medical help. Another study conducted by the Kaiser Family Foundation found that people with an income two times less than the federal poverty level used an average of 14% of their family’s income to pay for medical services, compared to 4.5% for those living with an income of at least four times that of the poverty level. Furthermore, the American Journal of Accountable Care found that rural and suburban areas were hindered by unaffordable medical care and relatively fewer primary care physicians.
Food deserts are an extensive and persistent problem, but people and organizations alike are working to find solutions. Community gardens, local farmers markets and growing public transportation are helping to eradicate food deserts. For example, nonprofit organizations like Meals on Wheels provide food to community members that need it.
In California, the CalFresh, or food stamps, program helps residents subsidize food costs. Moreover, California and other states participate in the Double Up Food Bucks program, which matches the amount that food stamps users pay, doubling the amount of groceries purchases.
Education can go a long way to help people in food deserts. Programs like Plan, Shop, Save and Cook from UC CalFresh Nutrition Education teach people how to make healthier choices. The federal Gus Schumacher Nutrition Incentive Program provides grants to organizations that promote vegetables and fruits purchases among underprivileged communities. Educational services with multilingual options also help immigrants and residents who don’t speak English.
Even small actions can prove invaluable. Raising awareness through posting on social media, volunteering at food banks and pantries and donating money and food are all ways community members can help. People can also learn more by subscribing to informational sites, such as Nourish California’s action alerts, about food legislation.
“I think the biggest thing to remember is that even in the wealthiest areas, there are still people that live under the poverty level and don’t have easy access to healthy foods,” Landry said. “Even though it might not be impacting you, there are still ways to help out because food access is just a basic human right.”